Metabolism Meltdown: Unraveling the Energy Crisis in Chronic Inflammatory Bowel Diseases
Chronic inflammatory bowel diseases (IBD), such as Crohn's disease and ulcerative colitis, cause recurring diarrhea, fever, pain, and significant psychological distress. Despite major advances and modern medications, treatment remains challenging. Only a subset of patients responds to medication.
A key issue in treating IBD is the profound disruption of the metabolic interaction between the body and the microbiome—the community of microbes residing in the gut. For the first time, this disruption has now been analyzed in detail by a research team from Kiel. The findings were published this week in the journal Nature Communications by scientists from the Faculty of Medicine at Kiel University and the University Medical Center Schleswig-Holstein (UKSH), Campus Kiel.
"Established IBD therapies typically target immune processes, as the diseases are driven by a misdirected immune response. However, since many patients do not respond adequately to these treatments, it is essential to understand disease mechanisms beyond the immune system—for example those at the metabolic level," explains Professor Christoph Kaleta from the Institute of Experimental Medicine (IEM) at Kiel University and UKSH, lead author of the study and member of the PMI Cluster of Excellence.
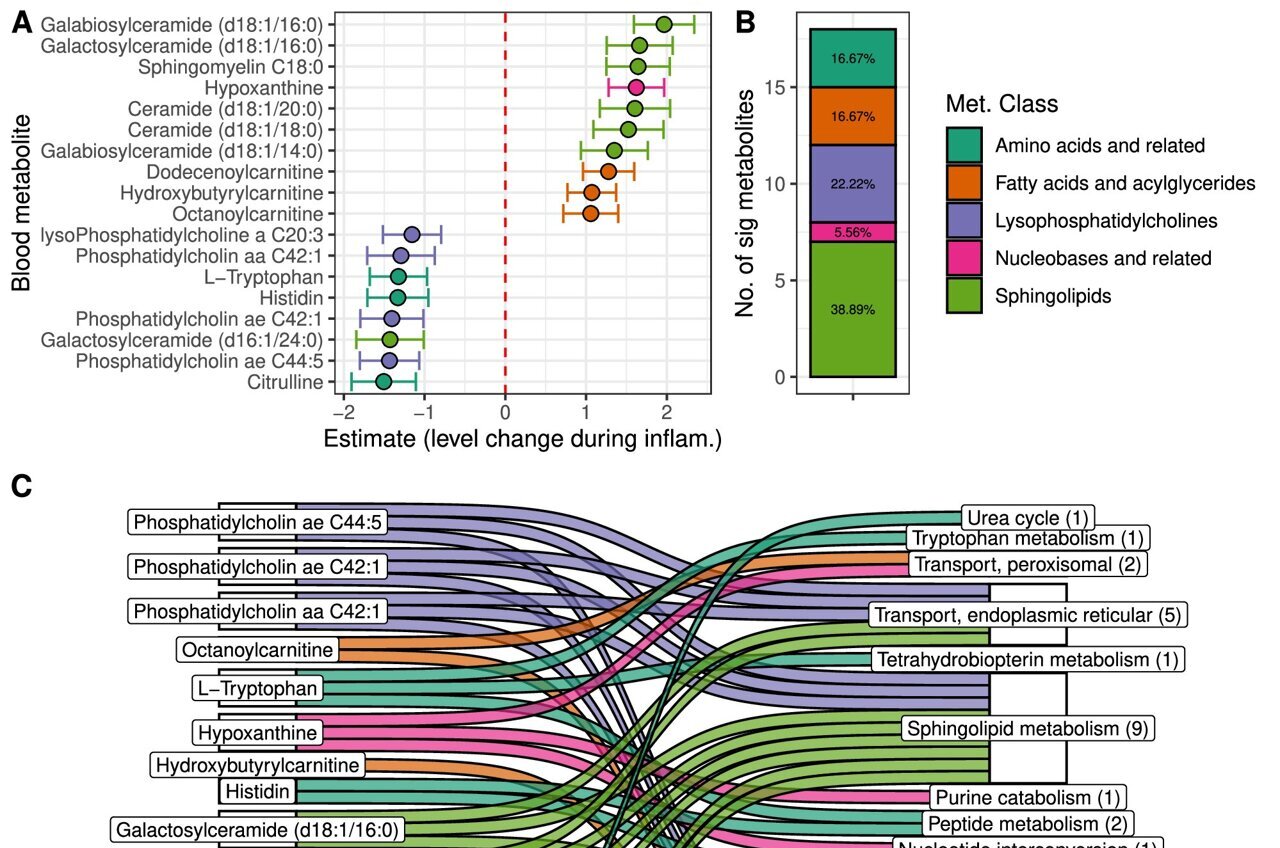
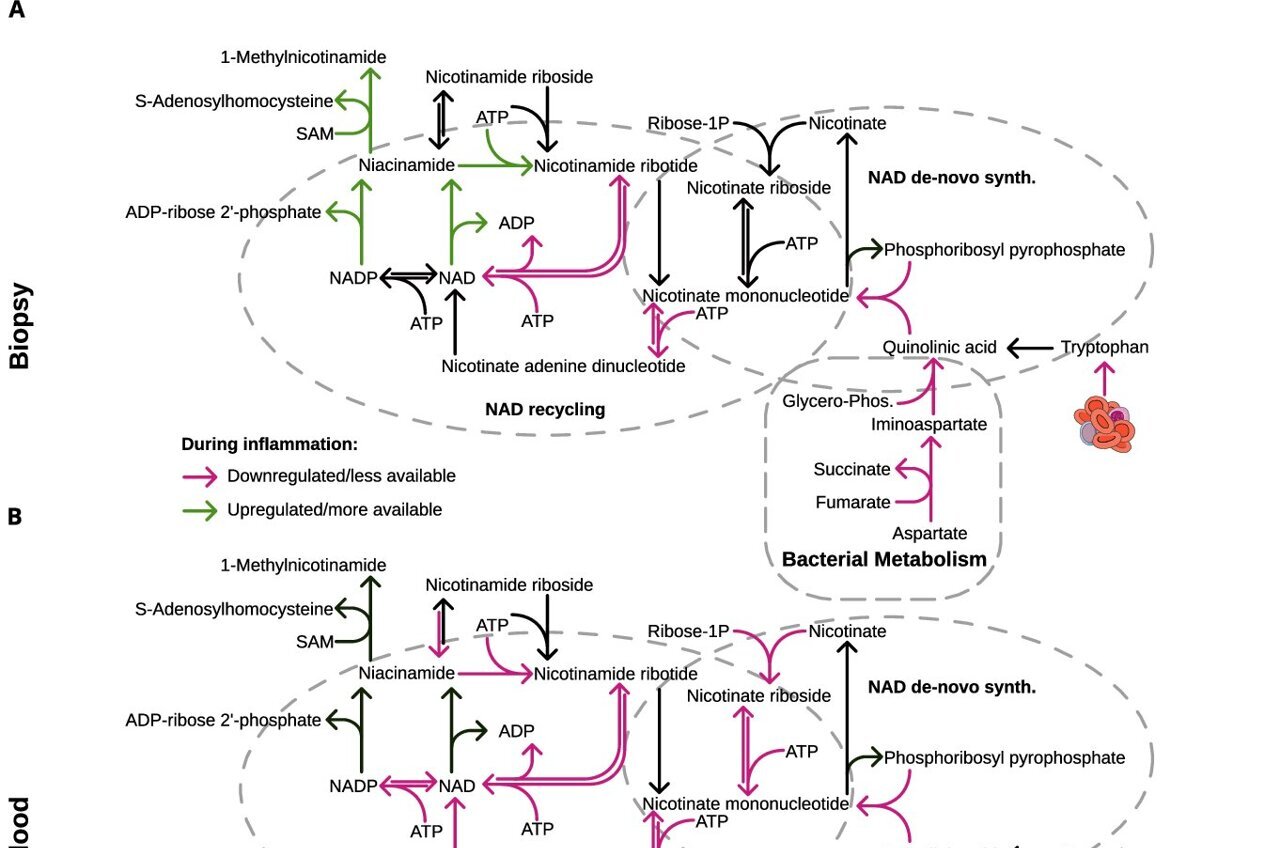
The researchers examined stool and blood samples from IBD patients before and after the start of therapy. They combined various molecular data—including metagenomics, transcriptomics, and metabolomics—with detailed computer-based network analyses to create a comprehensive picture of the patients' metabolic processes. Their key finding: metabolic activity in both the intestinal tissue and the gut microbiome is drastically reduced—and closely interlinked.
Energy supply and communication between host and microbiome collapse
"We were able to show that IBD leads to a breakdown in metabolic interactions between the host and the microbiome," says Kaleta. "This disrupted communication contributes to the failure of vital protective mechanisms and further exacerbates inflammation."
The team observed, among other things, that certain metabolic products—such as tryptophan and choline—were significantly reduced in the patients' blood. These substances are essential for producing the cells' key energy carriers, NAD and ATP. At the same time, bacterial metabolism of amino acids and dietary fibers also changed, reducing the production of metabolites which are normally used as energy sources by intestinal cells.
"Our results show that due to reduced metabolic performance, the microbiome produces fewer essential nutrients. As a result, human intestinal and immune cells must adjust their own metabolism. This causes an imbalance in both metabolism and the immune system, making treatment of these diseases particularly complex," explains Dr. Jan Taubenheim, first author of the study and postdoctoral researcher at the IEM.
Personalized nutrition as part of therapy
In an exploratory part of the study, the researchers used computer models to simulate whether targeted dietary changes—such as reducing certain carbohydrates or amino acids—could help restore the disturbed metabolic balance.
"Our simulations suggest that a targeted change in diet could alter the microbiome and thereby slow down inflammation-promoting metabolic processes," says Dr. Samer Kadib Alban, another first author of the study. "However, our results also show that there is no one-size-fits-all diet that effectively reduces inflammation. Nutrition needs to be tailored to each patient's metabolic profile."
"This study forms the basis for a better understanding of metabolic changes in IBD patients," Taubenheim continues. The next step will be to test these findings in the lab and develop specific therapies to counteract the metabolic disruptions.
The goal is to translate interdisciplinary research findings on chronic inflammatory diseases of barrier organs to health care more intensively, as well as to fulfill previously unsatisfied needs of the patients. Three points are important in the context of successful treatment, and are therefore at the heart of PMI research: the early detection of chronic inflammatory diseases, the prediction of disease progression and complications, and the prediction of individual responses to treatment.
More information: Jan Taubenheim et al, Metabolic modeling reveals a multi-level deregulation of host-microbiome metabolic networks in IBD, Nature Communications (2025). DOI: 10.1038/s41467-025-60233-2
Provided by Exzellenzcluster Präzisionsmedizin für chronische Entzündungserkrankungen
This story was originally published on Medical Xpress . Subscribe to our newsletter for the latest sci-tech news updates.
Post a Comment